I have just returned from India after a two-week stay in Bihar, one of the least developed state in this South Asian country [1]. Like many travellers from more developed countries, myself and my travel companions, one-by-one, developed diarrhoea after some times. Not surprisingly, since diarrhoea is one of the most common illnesses in travellers.

Traveller’s diarrhoea (TD) is, in fact, an accepted medical term. Up to 50% of individuals travelling to high-risk regions of tropical or semitropical regions develop diarrhoea [2]. Furthermore, travelling to South Asia carries the highest risk of developing diarrhoea syndromes compared to other parts of the world [3]. Acute and chronic diarrhoea account for almost 50% (456 out of every 1000 diagnosed cases) of the diagnosis of all returning travellers from the South Asian continent seeking medical attention. This is based on an analysis of the GeoSentinel database, a global network of clinics sharing data about travel-related illnesses [4].
This wasn’t my first visit to India. 10 years ago, during my first trip to India, acute diarrhoea and vomiting caused me to be bedridden for four full days. I had better knowledge and more prepared to handle TD this time round. The current medical advice for the prevention and treatment of TD is through the use of antibiotics, including ciprofloxacin (or levofloxacin), rifaximin, or azithromycin [2]. I hope to avoid the use of any antibiotics as much as I can. If you are like me, you will find the following tips to prevent and treat TD using natural remedies useful.
Prevention
Personal hygiene and dietary avoidance
More than 60% of the TD cases are caused by diarrhoea-producing bacteria such as Escherichia coli, Shigella, Campylobacter, Salmonella, Aeromonas, Plesiomonas, and noncholera Vibrios [2]. The disease is normally acquired through ingestion of contaminated food, water or other liquids [5]. Hence, practicing good personal hygiene and avoidance of high-risk foods and drinks is the first line of defence against TD.
Here are some prevention tips:
- Always wash your hands properly before meal or handling any foods or drinks, even though you are not touching the foods directly with your bare hand. (For more details on proper hand washing, please see “Keep Your Hands Clean” on Singapore Health Hub website [6].)
-

Drink only good quality bottled water with intact seal is a good practice while travelling. Always keep a hand sanitizer handy to disinfect your hand, even after proper hand washing.
- Some generally accepted advices on food and beverage selection include [7,8]:
- Avoid raw fruits and vegetables with intact skins, such as berries, tomatoes, and salads
- Avoid moist foods served at room temperature, including any food served buffet-style that is maintained at room temperature, or leftover food – Eat only food and beverage served steaming hot.
- Beware of non-pasteurized milk and other dairy products, they also can be of high risk.
- Never drink tap water, even in hotels claiming filtration systems – only drink good quality bottled water with intact seal.
- No ice please, even in alcoholic drinks
- Do not eat food from street vendors – extreme high risk of contamination

Use of probiotics
The caution in food and beverage selection cannot totally prevent TD, according to the latest systematic review published in The Journal of the American Medical Association (JAMA) [9]. Only a minority of travellers strictly adheres to all restrictive recommendations. After all, what’s the fun of travelling without being a little bit adventurous in sampling the local cuisine? Therefore, more preventive measures should be taken.
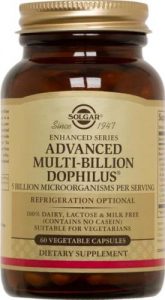
Probiotics supplements, especially those containing Saccharomyces boulardii and a mixture of Lactobacillus acidophilus and Bifidobacterium bifidum, have been shown to significantly prevent up to 85% of TD cases. This is according to a meta-analysis of twelve (12) randomized controlled studies published between 1997 to 2005 [5]. Probiotics can prevent TD because the microflora in our digestive tract is disrupted during travel. The normally protective bacteria in the intestines are disturbed by stress, jet lag, unfamiliar food and water and disrupted body rhythms, resulting in the weakening of the body’s normal defensive mechanisms against infections. Probiotics supplementation helps to restore the microflora environment, inhibit pathogen attachment, and enhance the immune response [10].
The efficacy of probiotics in the prevention of TD is accepted medically. The latest clinical recommendation is to start probiotics supplementation (Lactobacillus rhamnosus or S. boulardii) 2-5 days before departure and continue till return [11]. Hence, it is a good idea to start taking probiotics before your trip as a preventive measure against TD.
Self-Treatment
TD can still strike even after we have taken all the preventive measures. This happens to me while I was in India. It was all well during the first week when I stick to only hotel foods. The moment I started to eat out, as well as preparing some meal myself, my stomach started to rumble and I felt bloated, I knew diarrhoea would come next.
The typical symptoms of TD are loose or watery stools, abdominal cramping (80% of the case), fever (10-25%), vomiting (20%), and having blood or mucus in the stool (5-10%). Don’t be alarmed if you developed these symptoms, most TD cases are mild, with four and five loose or watery stools a day with little to no fever being the norm. Even without treatment, the diarrhoea usually lasts for only 3 to 4 days before resolving spontaneously in most cases [8]. The following self-treatment tips can help to reduce the severity of the symptoms, avoid significant disruption to your travel plan, and prevent post-TD complications.
Addressing the associating symptoms

The prelude to the development of diarrhoea is normally abdominal cramping. Nausea, vomiting and fever may follow suit. Try not to eat anything, including the probiotics supplement, during this stage as your digestive system may not be able to fully digest and absorb any nutrients; worse still, eating may further aggravate the symptoms. You likely will not have the appetite anyway. Restriction of fluid intake is also recommended.
Peppermint essential oil can be useful for easing the discomfort of abdominal cramping. Extensive research has been done on evaluating the efficacy of peppermint essential oil in improving abdominal pain, especially among patients with irritable bowel syndrome (IBS). This is confirmed by a systematic review and meta-analysis of nine (9) randomised, placebo-controlled trials that evaluated 726 patients [12]. Peppermint oil, which exert strong antimicrobial property against oral pathogens, may also eradicate bacteria causing TD [13]. In addition, peppermint oil may help to prevent or reduce fever, as well as relaxing the nervous system [14]. Furthermore, inhaling peppermint oil also helps to address nausea and prevent vomiting [15].
For the relieving of abdominal cramping and fever, here are a few ways to use peppermint oil:
- Inhale peppermint oil
- Apply topically on stomach and forehead
- Add a few drops into a small cup of hot water and slowly sip the mixture
- Add 5 to 10 drops in a capsule and take one capsule every 4 to 6 hours (for more serious cases with fever)

Stopping the diarrhoea
Don’t try to stop the diarrhoea immediately the moment you notice the loose stool. It is fine to have a few loose stools to let the body purge out all the faeces. Treat it as a form of detoxification and cleanse. After all, there are people who pay to get diarrhoea through methods such as colonic cleansing, even though there is no scientific evidence supporting its health benefits [16]. Abdominal pain and cramping will normally ease after several loose stools. You may also feel lighter. Stay in your hotel room, just take as much rest as you can.
If you stop eating any solid food when the symptoms developed, the discharge will quickly become watery. This is the time to stop the diarrhoea. I recommend a cup of hot black tea mix with ginger and molasses. A remedy that will stop the diarrhoea at this stage and help the digestive system to recuperate.

Tea (Camellia sinensis) extract has an effect on stopping diarrhoea due to its tannic acid content which inhibits the intestinal chloride (Cl–) secretion that lead to the physiological development of diarrhoea [17,18]. In addition, tea also contains organic components (catechins and theaflavins) that are known to be able to fight against disease-causing pathogens. In particular, the Epigallocatechin-3-gallate (EGCG) compound in tea is the most effective catechin that can destroy E. coli, the primary cause of TD [18].
Ginger (Zingiber officinale) is a traditional herb indicated for the treatment of many gastrointestinal diseases, including diarrhoea. Zingerone is the active compound in ginger that has anti-diarrhoeal activities such as stopping the contraction at the ileum of the colon [18]. Ginger is also an excellent anti-inflammatory and anti-microbial herb that can reduce any inflammation in the colon due to the bacteria infection [19]. Ginger can also improve nausea, ease abdominal bloating, and strengthen the digestive systems [20].
Molasses is the by-product of sugar production. However, unlike refined white sugar, which is empty calories depleted of all nutritional values, molasses is rich in mineral, especially calcium, magnesium, potassium, iron and manganese [21]. The body requires energy as well as electrolytes after fasting and diarrhoea. Molasses is ideally suited for replenishment and rehydration at this stage. In traditional Chinese medicine, ginger and molasses drink is a common folk prescription for strengthening the body, especially for weak and cold physique [22].

For me, the hot black tea with ginger and molasses beverage worked wonders during my last trip. The diarrhoea stopped overnight. The next morning, I felt hungry and my appetite was back. A good sign indicating the digestive system is making a recovery.
Making recovery

The first meal to break the fast after diarrhoea should be a semi-fluid diet. Rice porridge/congee with some boiled vegetables is recommended. It helps to rehydrate the body, provides the necessary nutrients, while not over stimulating the digestive systems. It is good to avoid meat, milk, dairy products, and gluten at this stage as they may irritate the bowel [23]. Avoid coffee, alcohol, carbonated or cold drinks as well. Your beverage of choice should be the hot black tea with ginger and molasses for the next few days. You should resume your probiotics supplementation as well. This is to restore the gut flora and strengthen the digestive tract.
About 10% of people who suffered from TD will develop post-infectious irritable bowel syndrome (PI-IBS), a chronic gastrointestinal disease with recurrent diarrhoea [24]. This may be due to the disruption and aggravation of the enteric nervous system that regulates the relaxation and contraction of the intestinal wall [25]. For prevention of such complication, the use of Iberogast®, an herbal formula for the treatment of IBS is recommended.

Iberogast® composed of nine herbs, including bitter Candytuft, Angelica, chamomile, caraway, milk thistle, lemon balm, peppermint, greater celandine, and liquorice [26]. These are carminative herbs known to relax the nervous system and digestive tract in Western herbalism, which have also been proven in a number of studies scientifically [27]. The product has been on the market for more than 30 years. A systematic review of 12 clinical trials using Iberogast® in functional dyspepsia (indigestive) and IBS since 1990 concluded that it is a safe and effective treatment that can help to reduce many gastrointestinal symptoms including abdominal pain, bloating, diarrhoea, etc. [28].
Hence, the use of Iberogast® after TD is recommended for two reasons. Firstly, it can help to reduce any further gastrointestinal symptoms not directly due to the infectious episode. Secondly, its effect on the enteric nervous system can help to quickly restore the balance of the gut-brain axis [29], preventing the development of PI-IBS. Take 20 drops of the herbal mixture in a small cup of water after every meal for the next 3 to 5 days, even if all the symptoms are gone.
Conclusion
TD is very common among travellers visiting less developed countries. Therefore, take all the precautions and be prepared to self-treat to minimise any discomfort and disruption to your trip.
Practicing good personal hygiene and avoidance of high-risk foods and drinks, such as raw foods, street foods, tap water, non-pasteurized milk and other dairy products can help to prevent TD to a certain extent. It is also prudent to start taking probiotics supplement 2-3 days before your trip and continue throughout your journey.
TD may not be fully prevented, so, get ready the following list of natural TD remedies in your travel pouch for self-treatment without depending on antibiotics:
- Peppermint essential oil – for easing symptoms, including abdominal cramping. Nausea, vomiting and fever
- Black tea – to stop the diarrhoea
- Ready mix ginger and molasses drink – reduce inflammation, rehydration, and restoration
- Iberogast – prevent against post-infection complication
- Probiotics – restoration of gut flora and immune system
With these remedies, you are well prepared for any TD episode.
Bon voyage!
References
[1] Odisha, Bihar least developed, Gujarat less developed: Raghuram Rajan panel – The Economic Times, (n.d.). http://economictimes.indiatimes.com/news/economy/indicators/odisha-bihar-least-developed-gujarat-less-developed-raghuram-rajan-panel/articleshow/23094215.cms (accessed December 21, 2016).
[2] J. de la Cabada Bauche, H.L. Dupont, New Developments in Traveler’s Diarrhea., Gastroenterol. Hepatol. (N. Y). 7 (2011) 88–95. http://www.ncbi.nlm.nih.gov/pubmed/21475415 (accessed December 21, 2016).
[3] D.R. Hill, N.J. Beeching, Travelersʼ diarrhea, Curr. Opin. Infect. Dis. 23 (2010) 481–487. doi:10.1097/QCO.0b013e32833dfca5.
[4] D.O. Freedman, L.H. Weld, P.E. Kozarsky, T. Fisk, R. Robins, F. von Sonnenburg, J.S. Keystone, P. Pandey, M.S. Cetron, Spectrum of Disease and Relation to Place of Exposure among Ill Returned Travelers, N. Engl. J. Med. 354 (2006) 119–130. doi:10.1056/NEJMoa051331.
[5] L. V. McFarland, Meta-analysis of probiotics for the prevention of traveler’s diarrhea, Travel Med. Infect. Dis. 5 (2007) 97–105. doi:10.1016/j.tmaid.2005.10.003.
[6] Keep Your Hands Clean, (n.d.). https://www.healthhub.sg/live-healthy/471/keepyourhandsclean (accessed December 21, 2016).
[7] H.L. DuPont, Systematic review: Prevention of travellers’ diarrhoea, Aliment. Pharmacol. Ther. 27 (2008) 741–751. doi:10.1111/j.1365-2036.2008.03647.x.
[8] D.J. Diemert, Prevention and self-treatment of traveler’s diarrhea, Clin. Microbiol. Rev. 19 (2006) 583–594. doi:10.1128/CMR.00052-05.
[9] R. Steffen, D.R. Hill, H.L. DuPont, Traveler’s Diarrhea, Jama. 313 (2015) 71. doi:10.1001/jama.2014.17006.
[10] L. MacFarland, G. Elmer, Probiotics of evidence-based probiotics for human health, in: I. Goktepe, V.K. Juneja, M. Ahmedna (Eds.), Probiotics Food Saf. Hum. Heal., CRC Press/Taylor & Francis, Boca Raton, FL, 2006: pp. 109–138. doi:10.1201/9781420027570.ch5.
[11] S.U. Islam, Clinical Uses of Probiotics., Medicine (Baltimore). 95 (2016) e2658. doi:10.1097/MD.0000000000002658.
[12] R. Khanna, J.K. MacDonald, B.G. Levesque, Peppermint Oil for the Treatment of Irritable Bowel Syndrome, J. Clin. Gastroenterol. 48 (2013) 1. doi:10.1097/MCG.0b013e3182a88357.
[13] N. Thosar, S. Basak, R.N. Bahadure, M. Rajurkar, Antimicrobial efficacy of five essential oils against oral pathogens: An in vitro study., Eur. J. Dent. 7 (2013) S71-7. doi:10.4103/1305-7456.119078.
[14] P. Mikaili, S. Mojaverrostami, M. Moloudizargari, S. Aghajanshakeri, Pharmacological and therapeutic effects of Mentha Longifolia L. and its main constituent, menthol., Anc. Sci. Life. 33 (2013) 131–8. doi:10.4103/0257-7941.139059.
[15] S. Tate, Peppermint oil: a treatment for postoperative nausea., J. Adv. Nurs. 26 (1997) 543–9. http://www.ncbi.nlm.nih.gov/pubmed/9378876 (accessed December 22, 2016).
[16] R.D. Acosta, B.D. Cash, Clinical Effects of Colonic Cleansing for General Health Promotion: A Systematic Review, Am. J. Gastroenterol. 104 (2009) 2830–2836. doi:10.1038/ajg.2009.494.
[17] M. Field, Intestinal ion transport and the pathophysiology of diarrhea., J. Clin. Invest. 111 (2003) 931–43. doi:10.1172/JCI18326.
[18] J.D. Dubreuil, Antibacterial and antidiarrheal activities of plant products against enterotoxinogenic Escherichia coli., Toxins (Basel). 5 (2013) 2009–41. doi:10.3390/toxins5112009.
[19] A. Saxena, K. Kaur, S. Hegde, F.M. Kalekhan, M.S. Baliga, R. Fayad, Dietary agents and phytochemicals in the prevention and treatment of experimental ulcerative colitis., J. Tradit. Complement. Med. 4 (2014) 203–17. doi:10.4103/2225-4110.139111.
[20] K. Bone, The Ultimate Herbal Compendium, Phytotherapy Press, Warwick, QLD, 2007.
[21] Molasses Nutrition Facts & Calories, (n.d.). http://nutritiondata.self.com/facts/sweets/5573/2 (accessed December 22, 2016).
[22] Z. Hai-Long, C. Shimin, L. Yalan, Some Chinese folk prescriptions for wind-cold type common cold., J. Tradit. Complement. Med. 5 (2015) 135–7. doi:10.1016/j.jtcme.2014.11.035.
[23] P.A. Hayes, M.H. Fraher, E.M.M. Quigley, Irritable bowel syndrome: the role of food in pathogenesis and management., Gastroenterol. Hepatol. (N. Y). 10 (2014) 164–74. http://www.ncbi.nlm.nih.gov/pubmed/24829543 (accessed December 22, 2016).
[24] E. Stermer, A. Lubezky, I. Potasman, E. Paster, A. Lavy, Is traveler’s diarrhea a significant risk factor for the development of irritable bowel syndrome? A prospective study., Clin. Infect. Dis. 43 (2006) 898–901. doi:10.1086/507540.
[25] B.G. Nezami, S. Srinivasan, Enteric nervous system in the small intestine: pathophysiology and clinical implications., Curr. Gastroenterol. Rep. 12 (2010) 358–65. doi:10.1007/s11894-010-0129-9.
[26] What is Iberogast?, (n.d.). http://iberogast.com.au/en/what-is-iberogast/ (accessed December 22, 2016).
[27] R. Rahimi, M. Abdollahi, Herbal medicines for the management of irritable bowel syndrome: a comprehensive review., World J. Gastroenterol. 18 (2012) 589–600. doi:10.3748/wjg.v18.i7.589.
[28] B. Ottillinger, M. Storr, P. Malfertheiner, H.-D. Allescher, STW 5 (Iberogast®)–a safe and effective standard in the treatment of functional gastrointestinal disorders., Wien. Med. Wochenschr. 163 (2013) 65–72. doi:10.1007/s10354-012-0169-x.
[29] M. Carabotti, A. Scirocco, M.A. Maselli, C. Severi, The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems., Ann. Gastroenterol. Q. Publ. Hell. Soc. Gastroenterol. 28 (2015) 203–209. http://www.ncbi.nlm.nih.gov/pubmed/25830558 (accessed December 22, 2016).
Great read, thankyou